
My 15 year old daughter loves soccer. She is known for her speed — she is super fast. Watching her sprint toward the goal and outrun the defense is exciting! She got to play on the varsity team her freshman year and even scored a few goals.
And then, one game mid-season, she seemed off. She looked pale. She was uncoordinated. She was tired. The next game, she was more tired, more pale. Other parents noticed how white her face looked out there against the green turf. She couldn’t run, her thighs were burning, her legs wouldn’t go.
“She’s anemic,” I said to myself. I knew it, but I didn’t know why.
Initial blood tests revealed some things:
- Red blood cell count was low
- Hemoglobin and hematocrit were low
- Total protein was low
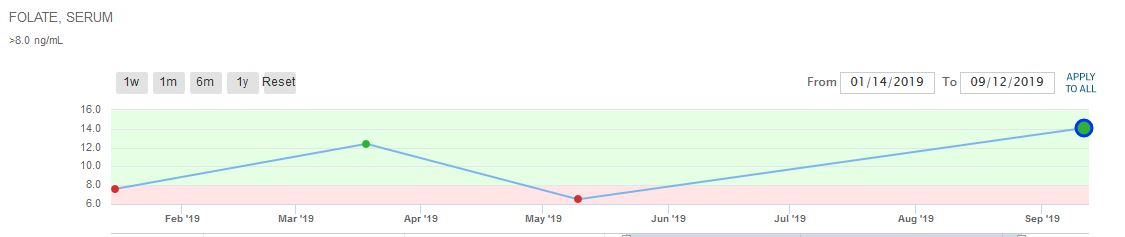
- Folate was low
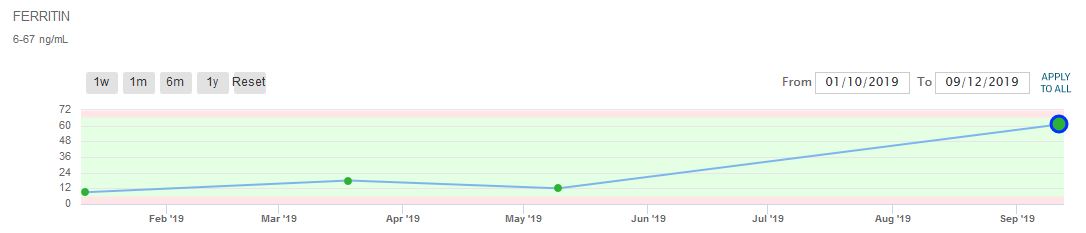
- Ferritin was in the normal range but on the low end
A stool sample showed blood in the stool. She was losing blood, resulting in the low blood cell count and other deficiencies. It was theorized that perhaps it was an ulcer, caused by taking Advil, which she had been routinely taking for the shin splints she was having. (I had already bought her new soccer shoes, and taken her to a podiatrist for insoles to help with the shin pain.) Could it really be ibuprofen causing her to bleed?
Both our pediatrician and the gastroenterologist we visited at UCSF seemed more interested in her family history — that is, me and my celiac diagnosis — than the Advil. I had raised her completely gluten-free but I knew that at some point she would want to eat gluten. I would pay attention to the common signs of celiac. Our house is 100% gluten-free so aside from the times she was out and about with her friends, I felt pretty confident that she was eating almost entirely gluten-free. (I would soon learn otherwise.)
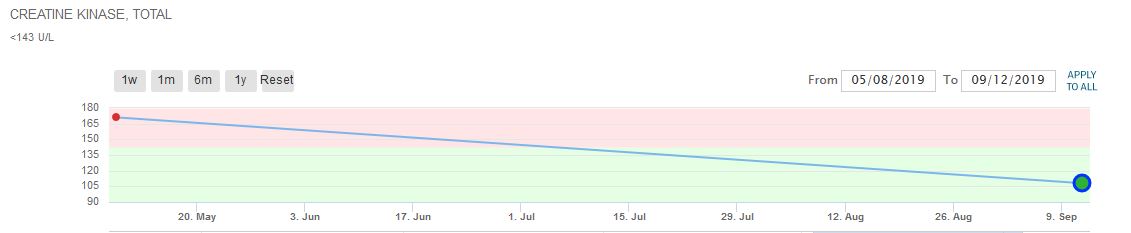
Another blood test revealed high creatine kinase (CK), which indicates muscle damage, and would make sense that every time she ran, her thighs were burning to the point that she had to ask the coach to take her out of the game after only a few minutes. In this condition, she had not performed well for the rest of the high school soccer season, and suffered through tryouts for club soccer. It was heart-breaking to see her decline.
And then, I took her to my long-time friend and colleague Sheila Wagner, now a naturopath, who has known my daughter since she was young. Sheila asked her: “What percent gluten-free are you?” My daughter answered: “70%.” I was shocked! I would have guessed 95%. Not that it matters, since celiac can be triggered by any amount, but if you never ate gluten, you would never develop celiac disease and all the problems that go with it. Sheila said, “I don’t think it’s an ulcer at all. I think it’s gluten.” Though I had talked to my daughter about celiac disease, it took another person — an authority figure other than me — to make her understand how it affects her. She presented in symptoms different from my own.
My daughter went 100% gluten-free, and also supplemented with iron and folate. Repeat tests showed no more blood in the stool. After three months, the true test would be a soccer tournament with her club team. With four games in one weekend, these would be the first games she would play since becoming totally gluten-free. Amazingly, she had no more leg pain! No more muscle fatigue! She played in all four games and scored goals for her team.
Looking back, I believe the shin pain was also a result of gluten and the vitamin deficiencies caused by gluten damage. She has not complained of shin pain since.
Her feeling better was validated by her blood tests taken three months after going gluten-free.
- Ferritin went from low 9 in January to high normal 61 in September (range is 6-67)
- Protein went in normal range
- Creatine Kinase went from high to normal
- Hemoglobin went from low 9.7 to normal 12.5 (range is 11.5 to 15.3)
- Hemotacrit went from low 28.6 to normal 37.1 (range is 34-46)
- Absolute eosinophils (Eosinophils become active when you have certain allergic diseases, infections, and other medical conditions) went from 416 to 46 (range 15-500)
- Folate went from low 6.5 to normal 14.1 (range is >8)
- Vitamin D crept into the normal range (no supplementation was given during this time)
This is a lot of specific information, but I love looking at blood test results over time — it is proof that diet affects the body. Inflammation and absorption can be measured.
The most satisfying results are seen in my daughter’s daily life. She has more energy, fewer headaches, no leg pain or muscle fatigue. She wakes up easier in the mornings and is less irritable. She never suffered the gastrointestinal effects of celiac disease like I did, but suffered in other ways. I am so happy to have her back.







Anna-Karen says
Alison, great input on your website.
I react to grains and probably have since childhood (fatigue, muscle pains, brain fog, stomach trouble, weak immune system, dry skin) but it was only two years ago that the onset of a terrible rash on my hands (dermatitis herpetiformis!) made me realise the connection to gluten/grains. It’s trial and error still, as other things like hazelnuts and preservatives are a problem,too, but websites such as yours are truly absolutely invaluable to get information, as doctors are basically hopeless.
My daughter is a peanut anaphylactic, my father had psoriasis as a child, and I do have slight vitiligo….
So thank you so so much for your efforts to put the information out there!!!
Alison says
Hi Anna-Karen,
Thank you for the nice note. It is interesting how all of these things are connected. Many dermatological conditions are connected but people don’t know it.